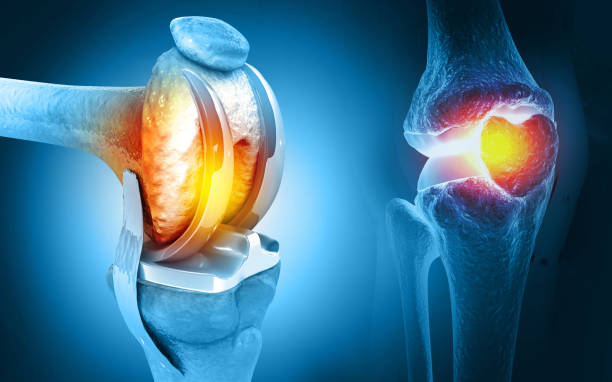
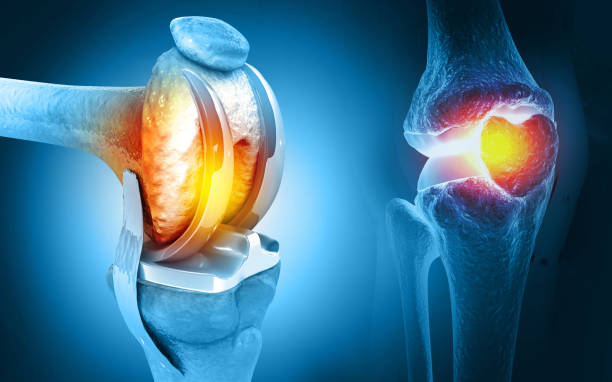
Knee prosthesis installation, commonly known as knee replacement surgery, is a crucial orthopedic procedure aimed at alleviating pain and restoring mobility for individuals suffering from severe knee conditions such as osteoarthritis or significant injuries.
In Turkey, this procedure is widely practiced with varying costs influenced by several key factors.
This extensive guide provides an in-depth exploration of the pricing dynamics and essential considerations associated with knee prosthesis installation across different cities in Turkey.
Factors Influencing Knee Prosthesis Installation Costs
The pricing of knee prosthesis installation in Turkey can vary significantly based on several critical factors that prospective patients should consider:
- Type of Knee Prosthesis: The cost of knee implants can vary based on the type chosen for the procedure. Standard implants, high-flexion implants allowing for greater range of motion, and custom-designed implants tailored to a patient’s unique anatomy all come with varying price points. Custom implants, though more expensive, may offer better long-term outcomes for some patients.
- Hospital Reputation and Facilities: Hospitals and clinics in Turkey differ in their reputation, facilities, and standards of care. Internationally accredited hospitals or those with advanced orthopedic departments tend to charge higher fees due to their superior infrastructure, quality of care, and experience in handling complex knee replacement surgeries.
- Surgeon’s Experience and Expertise: The proficiency and reputation of the orthopedic surgeon performing the procedure play a significant role in cost determination. Surgeons with extensive experience and specialized training in knee replacement surgery generally command higher fees, reflecting their skill level and success rates.
- Geographical Location: The city where the procedure is performed also influences pricing. Major urban centers like Istanbul, Ankara, and Izmir typically have higher living costs and demand for healthcare services, resulting in higher average procedure costs compared to smaller cities or rural areas in Turkey.
- Additional Costs: Beyond the surgery itself, additional costs can include pre-operative assessments, post-operative care such as physical therapy sessions, medication, and any unforeseen complications that may arise.
Prices of all types of the installation of a knee prosthesis procedure in Turkey.
Total Knee Replacement (TKR)
Definition and Details:
Total Knee Replacement (TKR), also known as total knee arthroplasty, is a surgical procedure designed to relieve pain and restore function in knees severely damaged by arthritis or injury.
It involves replacing the entire knee joint with artificial components made of metal alloys and high-grade plastics.
The procedure is typically recommended when non-surgical treatments like medications, physical therapy, and lifestyle modifications no longer provide adequate relief.
TKR aims to improve mobility, enhance joint function, and alleviate pain, thereby significantly improving the quality of life for patients suffering from advanced knee degeneration.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $200 – $500
- Comprehensive evaluation by orthopedic specialists, including physical exams, X-rays, MRI scans, and blood tests to assess the knee joint’s condition and overall health. Consultations with anesthesiologists and cardiologists may be required to ensure the patient is fit for surgery.
Surgical Procedure
- Cost: $3,000 – $5,000
- The surgical team administers anesthesia and makes an incision to access the knee joint. The damaged portions of the femur, tibia, and patella are carefully removed, and the surfaces are reshaped to fit the prosthetic components. Metal implants are secured to the ends of the femur and tibia, while a plastic spacer is inserted between them to recreate the smooth gliding motion of a healthy knee joint.
Implant Cost
- Cost: $2,500 – $7,000
- The total cost of knee implants varies depending on the type and quality of materials used. Standard implants are more affordable, while high-flexion implants allow for greater range of motion, and custom implants are designed to fit the patient’s unique anatomy. Implant costs typically include components for both the femoral and tibial sides, along with the patellar component if necessary.
Hospital Stay
- Cost: $1,000 – $3,000
- Covers admission, pre-operative preparation, surgical recovery room use, and inpatient care following surgery. Costs may vary based on the hospital’s facilities and the duration of the stay required for rehabilitation and monitoring.
Physical Therapy and Rehabilitation
- Cost: $500 – $1,500
- Essential for post-operative recovery, physical therapy sessions focus on strengthening muscles around the knee, improving flexibility, and restoring range of motion. Rehabilitation costs include sessions conducted both in the hospital and on an outpatient basis after discharge.
Medication
- Cost: $100 – $300
- Includes medications administered during hospitalization and prescribed for pain management, infection prevention, and blood clot prevention during the initial recovery phase. Costs may vary based on the duration of medication required and any adverse reactions that necessitate adjustments in treatment.
Follow-up Care
- Cost: $200 – $500
- Post-operative follow-up visits with orthopedic surgeons and physical therapists ensure proper healing and address any concerns or complications that may arise. Costs may include wound care, suture removal, and imaging studies to assess implant placement and bone integration.
Miscellaneous Costs
- Cost: $200 – $500
- Additional expenses may include diagnostic tests, such as X-rays or CT scans, to monitor post-operative healing and evaluate joint function. Costs also encompass durable medical equipment, such as knee braces or walkers, prescribed to support mobility during the recovery period.
Partial Knee Replacement (Unicondylar Knee Replacement)
Definition and Details:
Partial Knee Replacement, also known as unicondylar knee replacement, is a surgical procedure indicated for patients with localized arthritis affecting only one compartment of the knee joint.
Unlike total knee replacement, which involves replacing the entire joint, partial knee replacement preserves healthy bone, cartilage, and ligaments in the unaffected areas.
This approach aims to retain more natural knee anatomy, potentially resulting in faster recovery, improved range of motion, and a more natural feel compared to total knee replacement.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $200 – $500
- Initial consultations with orthopedic surgeons involve a comprehensive review of medical history, physical examination, and imaging studies (X-rays, MRI) to confirm the diagnosis of localized arthritis and assess joint integrity. Pre-operative evaluations may include consultations with anesthesiologists and cardiologists to optimize perioperative care and minimize surgical risks.
Surgical Procedure
- Cost: $2,500 – $4,500
- Anesthesia is administered, and a smaller incision is made to access the affected compartment of the knee joint. The damaged cartilage and bone are carefully removed from the femur and tibia, and the corresponding surfaces are prepared to accommodate the prosthetic components. A metal implant is secured to one side of the joint, while a plastic spacer is inserted to facilitate smooth articulation between the metal surfaces. The patella (knee cap) remains intact, preserving its natural function and alignment.
Implant Cost
- Cost: $2,000 – $6,000
- The cost of partial knee implants varies based on the type and design chosen by the surgeon. Standard implants are cost-effective but may offer limited customization, while high-flexion implants allow for greater range of motion and improved joint stability. Custom-designed implants are tailored to fit the patient’s specific anatomy, offering enhanced comfort and longevity. Implant costs typically include components for both the femoral and tibial sides, ensuring optimal alignment and function within the preserved knee compartment.
Hospital Stay
- Cost: $800 – $2,000
- Inpatient hospitalization covers admission, surgical recovery room use, and post-operative monitoring to ensure early mobilization and pain management. Costs may vary depending on the duration of hospitalization required for rehabilitation and the availability of specialized nursing care to facilitate recovery and minimize complications.
Physical Therapy and Rehabilitation
- Cost: $400 – $1,200
- Post-operative rehabilitation focuses on strengthening muscles around the knee, improving joint flexibility, and restoring functional mobility. Physical therapy sessions are tailored to the patient’s specific needs and may include exercises to enhance proprioception, balance, and coordination. Rehabilitation costs encompass both inpatient and outpatient sessions conducted under the guidance of experienced therapists to optimize recovery outcomes and facilitate a safe return to daily activities.
Medication
- Cost: $80 – $250
- Prescribed medications include pain relievers, antibiotics, and thromboprophylaxis agents administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of deep vein thrombosis (DVT) or pulmonary embolism (PE). Adjustments in medication dosages or formulations may be necessary based on individual patient responses and clinical indications, with ongoing monitoring to ensure therapeutic efficacy and safety throughout the recovery process.
Follow-up Care
- Cost: $160 – $400
- Post-operative follow-up visits with orthopedic surgeons are scheduled to evaluate surgical outcomes, monitor healing progress, and address any concerns or complications that may arise. Follow-up care includes wound assessments, suture removal, and imaging studies (X-rays, CT scans) to assess implant stability and joint function. Costs associated with follow-up visits may vary depending on the frequency of appointments and the need for diagnostic testing to guide clinical decision-making and optimize long-term joint health.
Miscellaneous Costs
- Cost: $160 – $400
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to assess pre-existing medical conditions and surgical risks. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to support post-operative recovery and promote functional independence. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and optimize overall wellness throughout the recovery journey.
Medial Pivot Knee Replacement
Definition and Details:
Medial Pivot Knee Replacement is a specialized type of total knee replacement (TKR) designed to replicate the natural movement and stability of the knee joint.
This implant design mimics the anatomy and biomechanics of a healthy knee, with a focus on improving functional outcomes and patient satisfaction.
The procedure is indicated for patients with degenerative knee conditions, such as osteoarthritis, requiring comprehensive joint reconstruction to alleviate pain and restore mobility.
Medial Pivot Knee Replacement offers enhanced stability during activities of daily living and functional movements, supporting a more natural gait pattern and joint alignment post-surgery.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $200 – $500
- Comprehensive evaluation by orthopedic specialists, including physical exams, imaging tests (X-rays, MRI scans), and laboratory studies to assess joint health and identify any pre-existing medical conditions. Consultations with anesthesiologists and other healthcare providers may be required to optimize perioperative care and manage potential surgical risks effectively.
Surgical Procedure
- Cost: $3,500 – $5,500
- Anesthesia is administered to ensure patient comfort during surgery, followed by a surgical incision to access the knee joint. The damaged surfaces of the femur, tibia, and patella are meticulously removed, and the bone is prepared to receive the prosthetic components. Medial Pivot Knee Replacement utilizes specialized implants designed to replicate the natural movement and stability of the knee joint, enhancing joint function and promoting long-term durability. The surgical team meticulously aligns and secures the implants to optimize joint mechanics and restore optimal range of motion for improved quality of life.
Implant Cost
- Cost: $3,000 – $7,000
- The cost of medial pivot knee implants varies based on the manufacturer, material composition, and technological advancements incorporated into the design. Standard implants offer cost-effective solutions for comprehensive joint reconstruction, while advanced models provide enhanced durability, biomechanical performance, and patient-specific customization options. Implant costs include components for the femoral, tibial, and patellar surfaces, ensuring optimal fit, alignment, and stability for reliable joint function and clinical outcomes.
Hospital Stay
- Cost: $1,200 – $3,000
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care to promote early mobilization and effective pain management. Costs associated with hospitalization may vary based on the duration of stay required for rehabilitation and the availability of specialized nursing care to support patient recovery and minimize complications. Inpatient services include monitoring vital signs, managing post-operative pain, and facilitating physical therapy sessions to enhance joint function and optimize recovery outcomes.
Physical Therapy and Rehabilitation
- Cost: $600 – $1,800
- Post-operative rehabilitation programs focus on restoring joint mobility, strengthening surrounding muscles, and improving functional abilities to support a return to daily activities. Physical therapy sessions are tailored to address individual patient needs and recovery milestones, incorporating therapeutic exercises, manual techniques, and modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing ongoing support and guidance to promote safe, effective recovery and achieve optimal outcomes following medial pivot knee replacement surgery.
Medication
- Cost: $120 – $400
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs vary based on the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support patient recovery throughout the rehabilitation process.
Follow-up Care
- Cost: $240 – $600
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor healing progress, and address any concerns or complications that may arise. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate implant positioning and joint function. Costs associated with follow-up appointments may vary depending on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and functional outcomes following medial pivot knee replacement surgery.
Miscellaneous Costs
- Cost: $240 – $600
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) conducted to evaluate pre-existing medical conditions and assess surgical risks. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Posterior-Stabilized Knee Replacement
Definition and Details:
Posterior-Stabilized Knee Replacement is a type of total knee arthroplasty designed to replace all components of the knee joint damaged by arthritis or trauma.
This surgical procedure aims to alleviate pain, restore mobility, and improve joint function by reconstructing the knee with specialized implants that replicate natural movement patterns and provide enhanced stability during various activities.
Posterior-stabilized knee implants feature an intercondylar notch and a cam mechanism to facilitate smooth flexion and extension motions while minimizing the risk of posterior instability and promoting optimal joint alignment.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $200 – $500
- Comprehensive evaluation by orthopedic specialists includes physical examinations, diagnostic imaging tests (e.g., X-rays, MRI scans), and laboratory studies to assess knee joint integrity and overall health status. Consultations with anesthesiologists and other medical providers ensure perioperative optimization and risk management strategies are implemented to enhance surgical outcomes and patient safety.
Surgical Procedure
- Cost: $3,200 – $5,200
- Anesthesia is administered to induce a state of unconsciousness and pain relief during surgery. A surgical incision is made to access the knee joint, and damaged bone and cartilage tissues are meticulously removed to prepare the femur, tibia, and patella for implant placement. Posterior-stabilized knee implants are selected based on patient-specific factors, including anatomical considerations, functional requirements, and desired surgical outcomes. The surgical team ensures precise alignment and secure fixation of implants to restore optimal joint function and facilitate early rehabilitation efforts.
Implant Cost
- Cost: $2,800 – $6,800
- The cost of posterior-stabilized knee implants varies depending on the manufacturer, material composition, and technological advancements incorporated into the implant design. Standard implants offer cost-effective solutions for comprehensive joint reconstruction, while advanced models provide enhanced durability, biomechanical performance, and patient-specific customization options. Implant costs encompass components for the femoral, tibial, and patellar surfaces to ensure optimal fit, alignment, and stability during post-operative recovery and functional rehabilitation.
Hospital Stay
- Cost: $1,100 – $2,800
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care to support early mobilization and effective pain management. Costs associated with hospitalization may vary based on the duration of stay required for rehabilitation and the availability of specialized nursing care to promote patient recovery and minimize potential complications. Inpatient services include monitoring vital signs, administering prescribed medications, and implementing physical therapy interventions to optimize joint function and facilitate safe discharge following posterior-stabilized knee replacement surgery.
Physical Therapy and Rehabilitation
- Cost: $550 – $1,650
- Post-operative rehabilitation programs focus on restoring joint mobility, strengthening surrounding musculature, and improving functional abilities to facilitate a safe return to daily activities. Physical therapy sessions are tailored to address individual patient needs and recovery milestones, incorporating therapeutic exercises, manual techniques, and modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing ongoing support and guidance to promote effective recovery and achieve favorable outcomes following posterior-stabilized knee replacement surgery.
Medication
- Cost: $110 – $350
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support patient recovery throughout the rehabilitation process.
Follow-up Care
- Cost: $220 – $550
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor healing progress, and address any concerns or complications that may arise. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate implant positioning and joint function. Costs associated with follow-up appointments may vary depending on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and functional outcomes following posterior-stabilized knee replacement surgery.
Miscellaneous Costs
- Cost: $220 – $550
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to evaluate pre-existing medical conditions and assess surgical risks. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Gender-Specific Knee Replacement
Definition and Details:
Gender-Specific Knee Replacement is a specialized form of total knee arthroplasty designed to address anatomical differences between male and female knee joints.
This surgical approach aims to optimize implant fit, alignment, and stability while accommodating gender-specific biomechanics and functional demands.
The procedure involves replacing damaged knee joint components with custom-designed implants tailored to meet the unique anatomical dimensions and alignment requirements of male and female patients.
Gender-specific knee replacements offer potential benefits, including improved joint function, enhanced durability, and reduced risk of implant-related complications, thereby supporting long-term mobility and quality of life for patients undergoing surgery.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $200 – $500
- Comprehensive evaluation by orthopedic specialists includes physical examinations, diagnostic imaging tests (e.g., X-rays, MRI scans), and laboratory studies to assess knee joint integrity and identify gender-specific anatomical variations. Consultations with anesthesiologists and other healthcare providers ensure perioperative optimization and risk management strategies are implemented to enhance surgical outcomes and patient safety.
Surgical Procedure
- Cost: $3,500 – $6,500
- Anesthesia is administered to induce a state of unconsciousness and pain relief during surgery. A surgical incision is made to access the knee joint, and damaged bone and cartilage tissues are meticulously removed to prepare the femur, tibia, and patella for implant placement. Gender-specific knee implants are selected based on patient-specific factors, including anatomical considerations, functional requirements, and desired surgical outcomes. The surgical team ensures precise alignment and secure fixation of implants to optimize joint function and facilitate early rehabilitation efforts.
Implant Cost
- Cost: $3,000 – $7,000
- The cost of gender-specific knee implants varies depending on the manufacturer, material composition, and technological advancements incorporated into the implant design. Custom-designed implants offer tailored solutions for comprehensive joint reconstruction, accommodating gender-specific anatomical variations and biomechanical characteristics. Implant costs encompass components for the femoral, tibial, and patellar surfaces to ensure optimal fit, alignment, and stability during post-operative recovery and functional rehabilitation.
Hospital Stay
- Cost: $1,200 – $3,000
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care to support early mobilization and effective pain management. Costs associated with hospitalization may vary based on the duration of stay required for rehabilitation and the availability of specialized nursing care to promote patient recovery and minimize potential complications. Inpatient services include monitoring vital signs, administering prescribed medications, and implementing physical therapy interventions to optimize joint function and facilitate safe discharge following gender-specific knee replacement surgery.
Physical Therapy and Rehabilitation
- Cost: $600 – $1,800
- Post-operative rehabilitation programs focus on restoring joint mobility, strengthening surrounding musculature, and improving functional abilities to facilitate a safe return to daily activities. Physical therapy sessions are tailored to address individual patient needs and recovery milestones, incorporating therapeutic exercises, manual techniques, and modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing ongoing support and guidance to promote effective recovery and achieve favorable outcomes following gender-specific knee replacement surgery.
Medication
- Cost: $120 – $400
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support patient recovery throughout the rehabilitation process.
Follow-up Care
- Cost: $240 – $600
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor healing progress, and address any concerns or complications that may arise. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate implant positioning and joint function. Costs associated with follow-up appointments may vary depending on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and functional outcomes following gender-specific knee replacement surgery.
Miscellaneous Costs
- Cost: $240 – $600
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to evaluate pre-existing medical conditions and assess surgical risks. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Unicompartmental (Partial) Knee Replacement
Definition and Details:
Unicompartmental Knee Replacement, also known as partial knee replacement, is a surgical procedure designed to replace only the damaged compartment of the knee affected by osteoarthritis or injury.
Unlike total knee replacement, which involves replacing all three compartments (medial, lateral, and patellofemoral), unicompartmental knee replacement preserves healthy bone and soft tissue structures in the unaffected parts of the knee.
This minimally invasive approach aims to alleviate pain, restore joint function, and improve mobility by replacing damaged cartilage and bone with specialized implants tailored to fit the specific anatomy and biomechanics of the affected knee compartment.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $200 – $500
- Comprehensive evaluation by orthopedic specialists includes physical examinations, diagnostic imaging tests (e.g., X-rays, MRI scans), and laboratory studies to assess knee joint integrity and determine the extent of compartmental damage. Patient-specific factors, including age, activity level, and overall health, are considered to determine candidacy for unicompartmental knee replacement surgery. Pre-operative planning ensures optimal implant selection, surgical approach, and perioperative care strategies to enhance surgical outcomes and patient satisfaction.
Surgical Procedure
- Cost: $3,000 – $6,000
- Anesthesia is administered to induce a state of unconsciousness and pain relief during surgery. A small incision is made to access the affected compartment of the knee joint, and damaged cartilage and bone tissues are carefully removed using specialized surgical instruments. Unicompartmental knee implants are meticulously positioned and secured to restore joint stability, facilitate smooth movement, and preserve healthy bone and soft tissue structures in the unaffected compartments. Surgical techniques aim to minimize trauma, accelerate recovery, and optimize functional outcomes for patients undergoing unicompartmental knee replacement surgery.
Implant Cost
- Cost: $2,500 – $5,500
- The cost of unicompartmental knee implants varies based on the manufacturer, material composition, and technological advancements incorporated into the implant design. Custom-designed implants offer tailored solutions for compartment-specific joint reconstruction, optimizing fit, alignment, and biomechanical performance. Implant costs encompass components for the femoral and tibial surfaces, ensuring precise articulation and stability during post-operative recovery and functional rehabilitation.
Hospital Stay
- Cost: $1,000 – $2,500
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care to support early mobilization and effective pain management. Costs associated with hospitalization may vary based on the duration of stay required for rehabilitation and the availability of specialized nursing care to promote patient recovery and minimize potential complications. Inpatient services include monitoring vital signs, administering prescribed medications, and implementing physical therapy interventions to optimize joint function and facilitate safe discharge following unicompartmental knee replacement surgery.
Physical Therapy and Rehabilitation
- Cost: $500 – $1,500
- Post-operative rehabilitation programs focus on restoring joint mobility, strengthening surrounding musculature, and improving functional abilities to facilitate a safe return to daily activities. Physical therapy sessions are tailored to address compartment-specific recovery goals, incorporating therapeutic exercises, manual techniques, and modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing ongoing support and guidance to promote effective recovery and achieve favorable outcomes following unicompartmental knee replacement surgery.
Medication
- Cost: $100 – $300
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support patient recovery throughout the rehabilitation process.
Follow-up Care
- Cost: $200 – $500
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor healing progress, and address any concerns or complications that may arise. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate implant positioning and joint function. Costs associated with follow-up appointments may vary depending on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and functional outcomes following unicompartmental knee replacement surgery.
Miscellaneous Costs
- Cost: $200 – $500
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to evaluate pre-existing medical conditions and assess surgical risks. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Revision Knee Replacement
Definition and Details:
Revision Knee Replacement is a complex surgical procedure performed to replace a previously implanted knee prosthesis that has become worn out, damaged, or infected over time.
This specialized orthopedic intervention aims to address complications associated with primary knee replacements, such as implant loosening, instability, or component failure, by removing the existing prosthesis and replacing it with new implants designed to restore joint function and alleviate symptoms.
Revision knee replacement requires meticulous pre-operative planning, intraoperative precision, and comprehensive post-operative care to optimize surgical outcomes and promote long-term joint health for patients experiencing recurrent knee joint issues.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $300 – $700
- Comprehensive evaluation by orthopedic specialists includes physical examinations, diagnostic imaging tests (e.g., X-rays, MRI scans), and laboratory studies to assess the condition of the existing knee prosthesis and identify underlying factors contributing to implant failure or complications. Patient-specific considerations, including medical history, implant longevity, and functional limitations, are evaluated to determine candidacy for revision knee replacement surgery. Pre-operative planning ensures appropriate implant selection, surgical approach, and perioperative management strategies to enhance surgical outcomes and minimize potential risks associated with revision knee replacement surgery.
Surgical Procedure
- Cost: $5,000 – $10,000
- Anesthesia is administered to induce a state of unconsciousness and pain relief during surgery. A surgical incision is made to access the knee joint, and the existing prosthetic components are carefully removed using specialized surgical instruments and techniques. Soft tissue structures, including ligaments and tendons, may require repair or reconstruction to optimize joint stability and ensure proper implant fixation. Revision knee implants are selected based on patient-specific factors, implant compatibility, and the extent of bone loss or structural deficiencies encountered during the surgical procedure. The surgical team utilizes advanced surgical techniques and technologies to achieve optimal implant positioning, restore joint function, and promote durable outcomes for patients undergoing revision knee replacement surgery.
Implant Cost
- Cost: $4,000 – $12,000
- The cost of revision knee implants varies depending on the manufacturer, material composition, and technological advancements incorporated into the implant design. Specialized implants offer advanced solutions for addressing complex joint reconstruction challenges, including bone defects, soft tissue deficiencies, and implant-related complications. Revision implant costs encompass components for the femoral, tibial, and patellar surfaces, ensuring comprehensive restoration of joint biomechanics, stability, and function during post-operative recovery and rehabilitation.
Hospital Stay
- Cost: $1,500 – $3,500
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care to support early mobilization and effective pain management. Costs associated with hospitalization may vary based on the duration of stay required for rehabilitation and the availability of specialized nursing care to promote patient recovery and minimize potential complications. Inpatient services include monitoring vital signs, administering prescribed medications, and implementing physical therapy interventions to optimize joint function and facilitate safe discharge following revision knee replacement surgery.
Physical Therapy and Rehabilitation
- Cost: $800 – $2,500
- Post-operative rehabilitation programs focus on restoring joint mobility, strengthening surrounding musculature, and improving functional abilities to facilitate a safe return to daily activities. Physical therapy sessions are tailored to address revision-specific recovery goals, incorporating therapeutic exercises, manual techniques, and modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing ongoing support and guidance to promote effective recovery and achieve favorable outcomes following revision knee replacement surgery.
Medication
- Cost: $150 – $500
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support patient recovery throughout the rehabilitation process.
Follow-up Care
- Cost: $300 – $750
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor healing progress, and address any concerns or complications that may arise. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate implant positioning and joint function. Costs associated with follow-up appointments may vary depending on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and functional outcomes following revision knee replacement surgery.
Miscellaneous Costs
- Cost: $300 – $750
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to evaluate pre-existing medical conditions and assess surgical risks. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Bilateral Knee Replacement
Definition and Details:
Bilateral Knee Replacement involves the simultaneous surgical replacement of both knee joints affected by severe osteoarthritis, rheumatoid arthritis, or other degenerative joint diseases.
This comprehensive orthopedic procedure aims to restore joint function, alleviate pain, and improve mobility by replacing damaged cartilage and bone with prosthetic implants tailored to each knee’s specific anatomical requirements.
Bilateral knee replacement surgery requires careful pre-operative planning, intraoperative coordination, and comprehensive post-operative rehabilitation to optimize surgical outcomes and facilitate simultaneous recovery for patients experiencing bilateral knee joint dysfunction.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $400 – $1,000
- Thorough evaluation by orthopedic specialists includes physical examinations, diagnostic imaging tests (e.g., X-rays, MRI scans), and laboratory studies to assess the condition of both knee joints and identify bilateral joint dysfunction. Patient-specific considerations, such as medical history, functional limitations, and overall health status, are evaluated to determine candidacy for bilateral knee replacement surgery. Pre-operative planning encompasses surgical risk assessment, implant selection, and perioperative management strategies to enhance surgical outcomes and ensure synchronized rehabilitation efforts for simultaneous bilateral knee replacement surgery.
Surgical Procedure
- Cost: $10,000 – $20,000
- Anesthesia is administered to induce a state of unconsciousness and pain relief during surgery. Simultaneous bilateral knee replacement surgery involves sequential surgical approaches to replace damaged cartilage and bone tissues in both knee joints. Orthopedic surgeons employ advanced surgical techniques and specialized instrumentation to ensure precise implant positioning, optimize joint alignment, and facilitate balanced limb function following bilateral knee replacement. Surgical interventions focus on restoring joint stability, promoting early mobilization, and minimizing intraoperative complications to achieve favorable outcomes for patients undergoing simultaneous bilateral knee replacement surgery.
Implant Cost
- Cost: $8,000 – $15,000 per knee
- The cost of bilateral knee implants varies based on the manufacturer, material composition, and technological advancements incorporated into the implant design. Prosthetic components for each knee joint include femoral, tibial, and patellar implants tailored to accommodate bilateral joint anatomy and biomechanical requirements. Bilateral implant costs encompass comprehensive joint reconstruction solutions, ensuring optimal fit, durability, and functional performance during post-operative recovery and rehabilitation following simultaneous bilateral knee replacement surgery.
Hospital Stay
- Cost: $3,000 – $6,000 per knee
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care for both knee joints to support simultaneous recovery and rehabilitation efforts. Costs associated with bilateral knee replacement surgery may vary based on the duration of hospitalization required, intensity of nursing care provided, and availability of specialized medical services to manage post-operative pain, promote joint mobility, and prevent potential complications. Inpatient services include continuous monitoring, administration of prescribed medications, and implementation of therapeutic interventions to optimize recovery outcomes for patients undergoing simultaneous bilateral knee replacement surgery.
Physical Therapy and Rehabilitation
- Cost: $1,500 – $3,000 per knee
- Post-operative rehabilitation programs focus on promoting bilateral knee joint mobility, enhancing muscular strength, and improving functional abilities to facilitate a coordinated return to daily activities. Physical therapy sessions are tailored to address bilateral joint-specific recovery goals, incorporating therapeutic exercises, manual techniques, and assistive modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing continuous support and guidance to promote effective recovery and achieve favorable outcomes following simultaneous bilateral knee replacement surgery.
Medication
- Cost: $300 – $600 per knee
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications following simultaneous bilateral knee replacement surgery. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support bilateral joint recovery throughout the rehabilitation process.
Follow-up Care
- Cost: $500 – $1,200 per knee
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor healing progress, and address any concerns or complications that may arise following simultaneous bilateral knee replacement surgery. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate implant positioning, joint alignment, and functional recovery for both knees. Costs associated with follow-up appointments may vary depending on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and bilateral functional outcomes.
Miscellaneous Costs
- Cost: $500 – $1,200 per knee
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to evaluate pre-existing medical conditions and assess surgical risks associated with bilateral knee replacement surgery. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence for both knees. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Complex (Multi-Ligament) Knee Reconstruction
Definition and Details:
Complex (Multi-Ligament) Knee Reconstruction is a specialized orthopedic procedure performed to repair or reconstruct multiple ligaments within the knee joint following traumatic injury, sports-related accidents, or severe degenerative joint disease.
This intricate surgical intervention aims to restore joint stability, optimize biomechanical function, and alleviate symptoms of instability or joint laxity by addressing concurrent ligamentous injuries affecting knee joint integrity.
Complex knee reconstruction requires meticulous pre-operative planning, intraoperative precision, and comprehensive post-operative rehabilitation to achieve optimal surgical outcomes and facilitate long-term joint health for patients experiencing complex knee joint issues.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $500 – $1,500
- Thorough evaluation by orthopedic specialists includes physical examinations, diagnostic imaging tests (e.g., X-rays, MRI scans), and arthroscopic assessments to assess the extent of ligamentous damage and identify concurrent knee joint injuries. Patient-specific considerations, such as injury mechanism, functional deficits, and previous surgical history, are evaluated to determine candidacy for complex knee reconstruction surgery. Pre-operative planning encompasses surgical risk assessment, ligament reconstruction strategies, and perioperative management strategies to enhance surgical outcomes and optimize joint stability for patients undergoing complex knee reconstruction.
Surgical Procedure
- Cost: $15,000 – $25,000
- Anesthesia is administered to induce a state of unconsciousness and pain relief during surgery. Complex knee reconstruction involves arthroscopic or open surgical approaches to repair or reconstruct multiple ligaments within the knee joint. Orthopedic surgeons utilize specialized techniques, including autograft or allograft tendon transfers, to restore ligamentous integrity and optimize joint biomechanics following traumatic knee injuries or chronic ligament laxity. Surgical interventions focus on achieving precise ligament tensioning, promoting graft integration, and facilitating early mobilization to enhance functional recovery and joint stability for patients undergoing complex knee reconstruction surgery.
Implant Cost
- Cost: $10,000 – $20,000
- The cost of complex knee reconstruction implants varies based on the type of graft material (e.g., autografts, allografts), implant fixation devices, and technological advancements incorporated into the surgical procedure. Graft options include hamstring tendons, patellar tendons, or cadaveric tissues sourced from tissue banks to facilitate ligamentous repair or reconstruction. Implant costs encompass comprehensive grafting solutions tailored to restore ligamentous function, optimize joint stability, and promote long-term biomechanical performance following complex knee reconstruction surgery.
Hospital Stay
- Cost: $5,000 – $10,000
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care to support complex knee reconstruction and facilitate early mobilization. Costs associated with hospitalization may vary based on the duration of stay required for rehabilitation, intensity of nursing care provided, and availability of specialized medical services to manage post-operative pain, promote joint mobility, and prevent potential complications. Inpatient services include continuous monitoring, administration of prescribed medications, and implementation of therapeutic interventions to optimize recovery outcomes for patients undergoing complex knee reconstruction surgery.
Physical Therapy and Rehabilitation
- Cost: $2,500 – $5,000
- Post-operative rehabilitation programs focus on restoring knee joint mobility, strengthening surrounding musculature, and enhancing functional abilities to facilitate a safe return to daily activities. Physical therapy sessions are tailored to address complex knee-specific recovery goals, incorporating therapeutic exercises, manual techniques, and assistive modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing continuous support and guidance to promote effective recovery and achieve favorable outcomes following complex knee reconstruction surgery.
Medication
- Cost: $500 – $1,000
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications following complex knee reconstruction surgery. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support ligamentous healing throughout the rehabilitation process.
Follow-up Care
- Cost: $600 – $1,500
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor ligamentous healing, and address any concerns or complications that may arise following complex knee reconstruction surgery. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate graft integrity, joint alignment, and functional recovery. Costs associated with follow-up appointments may vary based on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and functional outcomes following complex knee reconstruction surgery.
Miscellaneous Costs
- Cost: $600 – $1,500
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to evaluate pre-existing medical conditions and assess surgical risks associated with complex knee reconstruction surgery. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence for patients undergoing complex knee reconstruction. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Partial Knee Replacement (Unicompartmental Knee Replacement)
Definition and Details:
Partial Knee Replacement, also known as Unicompartmental Knee Replacement, is a surgical procedure designed to selectively replace only the damaged portion of the knee joint affected by localized osteoarthritis or degenerative joint disease.
This minimally invasive orthopedic intervention preserves healthy ligaments and bone structures in non-affected knee compartments, facilitating rapid recovery, reduced post-operative pain, and improved joint function compared to total knee replacement surgery.
Partial knee replacement is indicated for patients with isolated knee joint compartmental osteoarthritis or specific ligamentous defects amenable to partial joint reconstruction, offering a less invasive surgical alternative and potential preservation of natural knee joint mechanics.
Procedure Steps:
Pre-operative Assessment and Planning
- Cost: $300 – $1,000
- Comprehensive evaluation by orthopedic specialists includes physical examinations, diagnostic imaging tests (e.g., X-rays, MRI scans), and arthroscopic assessments to assess the extent of knee joint compartmental damage and confirm candidacy for partial knee replacement surgery. Patient-specific considerations, such as medical history, functional limitations, and overall health status, are evaluated to determine eligibility for partial knee replacement and optimize surgical outcomes. Pre-operative planning involves surgical risk assessment, implant selection, and perioperative management strategies to enhance joint-specific rehabilitation and facilitate personalized care for patients undergoing partial knee replacement surgery.
Surgical Procedure
- Cost: $8,000 – $15,000
- Anesthesia is administered to induce a state of unconsciousness and pain relief during surgery. Partial knee replacement involves arthroscopic or open surgical approaches to selectively replace damaged articular surfaces within a single knee joint compartment. Orthopedic surgeons utilize specialized instrumentation and implant components tailored to address localized osteoarthritic changes, restore joint biomechanics, and optimize functional outcomes following partial knee replacement surgery. Surgical interventions focus on preserving healthy knee joint structures, minimizing tissue trauma, and promoting rapid recovery with reduced post-operative pain compared to total knee replacement procedures.
Implant Cost
- Cost: $6,000 – $12,000
- The cost of partial knee replacement implants varies based on the manufacturer, implant design (e.g., fixed-bearing, mobile-bearing), and technological advancements incorporated into the implant components. Prosthetic implants for partial knee replacement include femoral, tibial, and patellar components customized to address specific knee joint compartmental defects and preserve natural knee mechanics. Implant costs encompass comprehensive joint reconstruction solutions aimed at restoring articular surface integrity, optimizing joint function, and promoting long-term biomechanical performance following partial knee replacement surgery.
Hospital Stay
- Cost: $2,000 – $5,000
- Inpatient hospitalization covers admission, surgical recovery room utilization, and comprehensive post-operative care following partial knee replacement surgery. Costs associated with hospitalization may vary based on the duration of inpatient stay required for rehabilitation, intensity of nursing care provided, and availability of specialized medical services to manage post-operative pain, promote joint mobility, and prevent potential complications. Inpatient services include continuous monitoring, administration of prescribed medications, and implementation of therapeutic interventions to optimize recovery outcomes for patients undergoing partial knee replacement surgery.
Physical Therapy and Rehabilitation
- Cost: $1,000 – $3,000
- Post-operative rehabilitation programs focus on restoring knee joint mobility, strengthening surrounding musculature, and enhancing functional abilities to facilitate a safe return to daily activities. Physical therapy sessions are tailored to address partial knee-specific recovery goals, incorporating therapeutic exercises, manual techniques, and assistive modalities to optimize musculoskeletal function and enhance overall well-being. Rehabilitation costs encompass both inpatient and outpatient services, providing continuous support and guidance to promote effective recovery and achieve favorable outcomes following partial knee replacement surgery.
Medication
- Cost: $200 – $500
- Prescribed medications include pain management agents, antibiotics, and thromboprophylaxis therapies administered during hospitalization and continued on an outpatient basis. Medication costs are influenced by the type, dosage, and duration of drug therapy required to manage post-operative pain, prevent infection, and minimize the risk of thromboembolic complications following partial knee replacement surgery. Pharmacological interventions are adjusted as needed to optimize therapeutic efficacy, mitigate adverse effects, and support joint-specific recovery throughout the rehabilitation process.
Follow-up Care
- Cost: $400 – $1,000
- Post-operative follow-up visits with orthopedic surgeons and allied health professionals are scheduled to assess surgical outcomes, monitor joint function, and address any concerns or complications that may arise following partial knee replacement surgery. Follow-up care includes wound assessments, suture removal, and diagnostic imaging studies (e.g., X-rays, CT scans) to evaluate implant positioning, joint alignment, and functional recovery. Costs associated with follow-up appointments may vary based on the frequency of visits and the need for additional medical interventions to optimize long-term joint health and functional outcomes following partial knee replacement surgery.
Miscellaneous Costs
- Cost: $300 – $750
- Additional expenses may include diagnostic tests (e.g., laboratory studies, imaging studies) performed to evaluate pre-existing medical conditions and assess surgical risks associated with partial knee replacement surgery. Costs associated with miscellaneous supplies (e.g., dressings, bandages) and durable medical equipment (e.g., assistive devices, mobility aids) prescribed to facilitate post-operative recovery and promote functional independence for patients undergoing partial knee replacement. Ancillary services, such as nutritional counseling and psychological support, may also incur additional costs to address holistic patient needs and enhance overall wellness throughout the rehabilitation journey.
Price Comparison of Knee Replacement Procedures in Istanbul, Ankara, and Izmir
Total Knee Replacement
Istanbul:
- Procedure Cost: $9,000 – $15,000
- Implant Cost: $4,000 – $8,000
- Hospital Stay: $3,000 – $5,000
- Physical Therapy: $1,500 – $3,000
- Medication: $300 – $600
- Follow-up Care: $500 – $1,200
Ankara:
- Procedure Cost: $8,000 – $14,000
- Implant Cost: $3,500 – $7,500
- Hospital Stay: $2,500 – $4,500
- Physical Therapy: $1,200 – $2,500
- Medication: $250 – $500
- Follow-up Care: $400 – $1,000
Izmir:
- Procedure Cost: $7,500 – $13,000
- Implant Cost: $3,000 – $6,500
- Hospital Stay: $2,000 – $4,000
- Physical Therapy: $1,000 – $2,000
- Medication: $200 – $400
- Follow-up Care: $300 – $800
Partial Knee Replacement (Unicompartmental Knee Replacement)
Istanbul:
- Procedure Cost: $8,000 – $15,000
- Implant Cost: $6,000 – $12,000
- Hospital Stay: $2,000 – $5,000
- Physical Therapy: $1,000 – $3,000
- Medication: $200 – $500
- Follow-up Care: $400 – $1,000
Ankara:
- Procedure Cost: $7,000 – $13,000
- Implant Cost: $5,500 – $10,000
- Hospital Stay: $1,500 – $4,000
- Physical Therapy: $800 – $2,000
- Medication: $150 – $400
- Follow-up Care: $300 – $800
Izmir:
- Procedure Cost: $6,500 – $12,000
- Implant Cost: $5,000 – $9,000
- Hospital Stay: $1,500 – $3,500
- Physical Therapy: $700 – $1,500
- Medication: $150 – $300
- Follow-up Care: $250 – $600
Revision Knee Replacement
Istanbul:
- Procedure Cost: $12,000 – $20,000
- Implant Cost: $8,000 – $15,000
- Hospital Stay: $4,000 – $7,000
- Physical Therapy: $2,000 – $4,000
- Medication: $400 – $800
- Follow-up Care: $600 – $1,500
Ankara:
- Procedure Cost: $11,000 – $18,000
- Implant Cost: $7,500 – $13,000
- Hospital Stay: $3,500 – $6,000
- Physical Therapy: $1,500 – $3,000
- Medication: $300 – $600
- Follow-up Care: $500 – $1,200
Izmir:
- Procedure Cost: $10,000 – $17,000
- Implant Cost: $7,000 – $12,000
- Hospital Stay: $3,000 – $5,000
- Physical Therapy: $1,200 – $2,500
- Medication: $250 – $500
- Follow-up Care: $400 – $1,000
Minimally Invasive Knee Replacement
Istanbul:
- Procedure Cost: $10,000 – $17,000
- Implant Cost: $6,500 – $12,000
- Hospital Stay: $3,500 – $6,000
- Physical Therapy: $1,500 – $3,000
- Medication: $300 – $600
- Follow-up Care: $500 – $1,200
Ankara:
- Procedure Cost: $9,000 – $15,000
- Implant Cost: $6,000 – $10,000
- Hospital Stay: $3,000 – $5,000
- Physical Therapy: $1,200 – $2,500
- Medication: $250 – $500
- Follow-up Care: $400 – $1,000
Izmir:
- Procedure Cost: $8,500 – $14,000
- Implant Cost: $5,500 – $9,500
- Hospital Stay: $2,500 – $4,500
- Physical Therapy: $1,000 – $2,000
- Medication: $200 – $400
- Follow-up Care: $300 – $800
Gender-Specific Knee Replacement
Istanbul:
- Procedure Cost: $9,500 – $16,000
- Implant Cost: $5,500 – $11,000
- Hospital Stay: $3,000 – $5,500
- Physical Therapy: $1,500 – $2,800
- Medication: $300 – $600
- Follow-up Care: $500 – $1,000
Ankara:
- Procedure Cost: $8,500 – $14,500
- Implant Cost: $5,000 – $10,000
- Hospital Stay: $2,500 – $4,500
- Physical Therapy: $1,200 – $2,500
- Medication: $250 – $500
- Follow-up Care: $400 – $800
Izmir:
- Procedure Cost: $8,000 – $13,500
- Implant Cost: $4,500 – $9,000
- Hospital Stay: $2,000 – $4,000
- Physical Therapy: $1,000 – $2,000
- Medication: $200 – $400
- Follow-up Care: $300 – $700
Robotic-Assisted Knee Replacement
Istanbul:
- Procedure Cost: $11,000 – $18,000
- Implant Cost: $7,000 – $13,000
- Hospital Stay: $4,000 – $6,500
- Physical Therapy: $1,800 – $3,500
- Medication: $400 – $800
- Follow-up Care: $600 – $1,200
Ankara:
- Procedure Cost: $10,000 – $16,000
- Implant Cost: $6,500 – $12,000
- Hospital Stay: $3,500 – $5,500
- Physical Therapy: $1,500 – $3,000
- Medication: $300 – $600
- Follow-up Care: $500 – $1,000
Izmir:
- Procedure Cost: $9,500 – $15,500
- Implant Cost: $6,000 – $11,000
- Hospital Stay: $3,000 – $5,000
- Physical Therapy: $1,200 – $2,500
- Medication: $250 – $500
- Follow-up Care: $400 – $800
Bilateral Knee Replacement
Istanbul:
- Procedure Cost: $18,000 – $30,000
- Implant Cost: $15,000 – $25,000 (for both knees)
- Hospital Stay: $6,000 – $10,000
- Physical Therapy: $3,000 – $6,000
- Medication: $600 – $1,200
- Follow-up Care: $1,000 – $2,400
Ankara:
- Procedure Cost: $16,000 – $28,000
- Implant Cost: $13,000 – $22,000 (for both knees)
- Hospital Stay: $5,000 – $9,000
- Physical Therapy: $2,500 – $5,000
- Medication: $500 – $1,000
- Follow-up Care: $800 – $2,000
Izmir:
- Procedure Cost: $15,000 – $26,000
- Implant Cost: $12,000 – $20,000 (for both knees)
- Hospital Stay: $4,500 – $8,000
- Physical Therapy: $2,000 -$4,500
- Medication: $400 – $900
- Follow-up Care: $700 – $1,800
Complex Knee Replacement
Istanbul:
- Procedure Cost: $20,000 – $35,000
- Implant Cost: $18,000 – $30,000
- Hospital Stay: $8,000 – $12,000
- Physical Therapy: $4,000 – $8,000
- Medication: $800 – $1,500
- Follow-up Care: $1,500 – $3,000
Ankara:
- Procedure Cost: $18,000 – $32,000
- Implant Cost: $16,000 – $28,000
- Hospital Stay: $7,000 – $10,000
- Physical Therapy: $3,500 – $7,000
- Medication: $700 – $1,300
- Follow-up Care: $1,200 – $2,500
Izmir:
- Procedure Cost: $17,000 – $30,000
- Implant Cost: $15,000 – $26,000
- Hospital Stay: $6,500 – $9,500
- Physical Therapy: $3,000 – $6,000
- Medication: $600 – $1,200
- Follow-up Care: $1,000 – $2,000
Patellofemoral Arthroplasty
Istanbul:
- Procedure Cost: $10,000 – $18,000
- Implant Cost: $7,000 – $13,000
- Hospital Stay: $3,500 – $6,500
- Physical Therapy: $1,800 – $3,500
- Medication: $400 – $800
- Follow-up Care: $600 – $1,200
Ankara:
- Procedure Cost: $9,000 – $16,000
- Implant Cost: $6,500 – $12,000
- Hospital Stay: $3,000 – $5,500
- Physical Therapy: $1,500 – $3,000
- Medication: $300 – $600
- Follow-up Care: $500 – $1,000
Izmir:
- Procedure Cost: $8,500 – $15,500
- Implant Cost: $6,000 – $11,000
- Hospital Stay: $2,500 – $5,000
- Physical Therapy: $1,200 – $2,500
- Medication: $250 – $500
- Follow-up Care: $400 – $800
Cartilage Restoration with Knee Replacement
Istanbul:
- Procedure Cost: $12,000 – $20,000
- Implant Cost: $9,000 – $16,000
- Hospital Stay: $4,000 – $7,000
- Physical Therapy: $2,000 – $4,000
- Medication: $400 – $800
- Follow-up Care: $600 – $1,500
Ankara:
- Procedure Cost: $11,000 – $18,000
- Implant Cost: $8,500 – $14,000
- Hospital Stay: $3,500 – $6,000
- Physical Therapy: $1,500 – $3,000
- Medication: $300 – $600
- Follow-up Care: $500 – $1,200
Izmir:
- Procedure Cost: $10,500 – $17,500
- Implant Cost: $8,000 – $13,500
- Hospital Stay: $3,000 – $5,500
- Physical Therapy: $1,200 – $2,500
- Medication: $250 – $500
- Follow-up Care: $400 – $1,000
Factors Influencing the Price Differences of Knee Replacement Procedures Between Istanbul, Ankara, and Izmir.
Medical Expertise and Reputation
- Surgeon Experience: Highly experienced surgeons with specialized training in knee replacement procedures often charge more. Istanbul, being a larger and more internationally renowned city, attracts top-tier medical professionals who have extensive experience and international certifications, contributing to higher costs. These surgeons might have decades of experience and a significant number of successful surgeries, often adding to their reputation and demand. Patients are often willing to pay a premium for the peace of mind that comes with knowing they are in the hands of one of the best surgeons available. Surgeons in Istanbul may have trained abroad and bring cutting-edge techniques and knowledge back to Turkey, enhancing their market value.
- Hospital Reputation: Hospitals in Istanbul, such as the American Hospital and Acıbadem Hospitals Group, are known for their high standards and cutting-edge facilities, which come at a premium. These hospitals often have accreditations from international health organizations, ensuring they meet stringent global standards. In contrast, hospitals in Ankara and Izmir, while still offering excellent care, may have lower operational costs, affecting the overall pricing. The reputation of these hospitals is built on years of consistent, high-quality care and often includes state-of-the-art facilities, highly trained staff, and a range of support services that justify their higher costs.
Technological Advancements
- Availability of Advanced Techniques: Istanbul is more likely to offer the latest technological advancements in knee replacement, such as robotic-assisted surgeries and minimally invasive techniques. These advanced procedures often require expensive equipment and specialized training, increasing the cost. For instance, robotic-assisted knee replacements offer higher precision and potentially better outcomes, but the initial investment in robotic systems is substantial. Hospitals in Istanbul are more likely to have the financial resources to invest in such technologies, which can be a significant factor in the higher costs.
- Infrastructure Investment: The level of investment in medical infrastructure, including state-of-the-art surgical suites and post-operative care facilities, is typically higher in Istanbul, leading to higher procedural costs. This includes everything from advanced imaging technologies to ensure accurate diagnostics and planning, to high-end surgical tools that provide better outcomes. Additionally, post-operative care facilities in Istanbul might offer a higher standard of care with more amenities, contributing to the overall expense. These investments ensure that patients receive the highest quality care, which is reflected in the pricing.
Economic Factors
- Cost of Living: Istanbul has a higher cost of living compared to Ankara and Izmir. This affects everything from staff salaries to the cost of utilities and medical supplies, contributing to higher medical bills. The cost of living in Istanbul influences the wages of medical staff, from surgeons and nurses to administrative and support staff, all of whom require competitive salaries to cope with the higher living expenses. Higher real estate costs in Istanbul also mean that hospital facilities, both in terms of land and maintenance, are more expensive, further pushing up the cost of medical services.
- Economic Status of Patients: Patients in Istanbul may have higher disposable incomes, allowing hospitals to charge more for procedures without significantly impacting demand. The city attracts a wealthier demographic, including both locals and international patients who are willing to pay for premium services. This economic dynamic allows hospitals to maintain higher prices while still operating at full capacity. Additionally, medical tourism contributes significantly to this, as international patients often come with the expectation of paying higher prices for what they perceive as superior care.
Geographic and Demographic Considerations
- Population Density: Istanbul’s large and densely packed population creates a higher demand for medical services, which can drive up prices. Higher demand can lead to longer waiting times and increased competition for available surgery slots, pushing prices up. In contrast, Ankara and Izmir, with their smaller populations, may have lower demand, influencing the pricing strategy. The high population density in Istanbul also means hospitals must cater to a large number of patients, requiring more staff, more extensive facilities, and more resources, all of which contribute to higher costs.
- Medical Tourism: Istanbul is a major hub for medical tourism. International patients seeking high-quality care are often willing to pay more, which can drive up prices for locals as well. Medical tourists are drawn to Istanbul for its renowned medical facilities, experienced surgeons, and the city’s cultural attractions. Hospitals often offer packages that include not just the medical procedure but also accommodation, transportation, and sometimes even sightseeing tours, adding to the overall cost. The influx of international patients, who typically have higher budgets, allows hospitals to charge premium rates.
Hospital and Facility Costs
- Operational Costs: Running a hospital in Istanbul, with its higher real estate and maintenance costs, is more expensive than in Ankara or Izmir. This includes everything from building leases to advanced medical equipment maintenance. Hospitals in Istanbul are likely to have larger, more modern facilities that require significant investment in maintenance and updates to keep up with technological advancements. Additionally, the costs of utilities such as electricity, water, and heating are higher in Istanbul, contributing to the overall operational expenses.
- Bed Occupancy Rates: Higher bed occupancy rates in Istanbul can lead to higher operational efficiency, but also higher prices due to demand. Hospitals in Istanbul might have higher turnover rates and need to accommodate more patients, leading to increased staffing needs and resource consumption. Lower occupancy rates in Ankara and Izmir can reduce costs but might also mean less revenue, which could lead to cost-cutting measures that affect pricing. The dynamic of bed occupancy also influences how hospitals manage their resources and pricing strategies to maximize profitability.
Market Competition
- Number of Hospitals and Clinics: Istanbul has a larger number of hospitals and clinics competing for patients, which can sometimes lead to competitive pricing. However, top-tier facilities still command higher prices.
- Quality of Competing Facilities: The presence of high-quality competing facilities can drive up standards and costs. In Istanbul, the competition among top-tier hospitals keeps the bar high, which is not always the case in Ankara and Izmir.
Patient Preferences and Demand
- Patient Preferences: Patients in Istanbul might prefer hospitals with more amenities and luxury services, contributing to higher costs. Preferences for private rooms, gourmet meals, and personalized care can all add to the bill.
- Seasonal Demand: The demand for medical procedures can vary seasonally. Istanbul, with its fluctuating medical tourist population, might experience seasonal price hikes.
Training and Education
- Access to Training Facilities: Proximity to leading medical universities and research institutions, more prevalent in Istanbul, means access to ongoing medical training and cutting-edge research, which can elevate the cost of procedures.
- Continuing Education: Surgeons and medical staff in Istanbul might have more opportunities for continuing education and training, contributing to higher costs due to their advanced skill levels.
Ancillary Services
- Post-operative Care: The quality and duration of post-operative care, including physical therapy and follow-up visits, can differ significantly. Istanbul’s higher costs often include comprehensive post-operative care packages.
- Support Services: Additional services such as patient counseling, nutritional support, and home care services are more readily available in Istanbul, contributing to the overall cost.
Understanding Variations in Hospital Pricing
The disparity in pricing between hospitals within Turkey can be attributed to several influencing factors:
- Hospital Type: Private hospitals generally charge higher fees compared to public or university-affiliated hospitals due to their premium services, state-of-the-art technology, and luxurious amenities.
- Facility Standards: Hospitals equipped with advanced surgical equipment and facilities for intensive care may justify higher costs to cover operational expenses and maintain quality standards.
- Location-specific Costs: Geographic factors such as real estate prices, utility costs, and local taxes contribute to varying pricing structures across different regions and cities in Turkey.
Additional Cost Considerations for Knee Prosthesis Installation
Consultation Fees: Initial consultations with orthopedic surgeons often involve separate fees, which may or may not be included in the overall surgical package.
- Diagnostic Tests: Essential diagnostic tests such as X-rays, MRI scans, and blood work are necessary pre-operative assessments to evaluate a patient’s candidacy for knee replacement surgery and incur additional costs.
- Physical Therapy and Rehabilitation: Post-operative rehabilitation is crucial for successful recovery and may involve multiple sessions with physical therapists. The cost of rehabilitation services should be factored into the overall budget for knee prosthesis installation.
- Medication and Disposables: Prescription medications for pain management, antibiotics, and medical supplies used during and after surgery are additional expenses not typically covered in the surgical package and should be accounted for separately.
Insurance Coverage and Payment Options
For patients considering knee prosthesis installation in Turkey, exploring insurance coverage options is essential:
- International Insurance Policies: Some private medical insurance plans may cover a portion or all of the expenses associated with knee replacement surgery in Turkey. Patients should verify coverage details, including any deductibles or co-payments.
- Direct Payment Options: Hospitals and clinics in Turkey often accept various payment methods, including major credit cards, wire transfers, and cash payments in multiple currencies such as USD, EUR, or GBP. Flexible payment plans may also be available to accommodate different financial situations.
Preparation Guide for Undergoing Knee Replacement Surgery.
Personal Preparations
Physical Conditioning:
- Exercise: Strengthening the muscles around your knee joint is vital. Engaging in low-impact exercises such as swimming, cycling, or walking can help improve your overall fitness and enhance recovery post-surgery. Exercises like leg lifts, hamstring curls, and quadriceps sets are particularly beneficial.
- Weight Management: Maintaining a healthy weight is crucial as it reduces the strain on your knee. If you are overweight, consider a weight loss plan to shed excess pounds. This not only improves surgical outcomes but also eases post-operative rehabilitation.
Diet and Nutrition:
- Balanced Diet: Eating a nutritious diet rich in vitamins, minerals, and proteins can boost your immune system and aid in faster recovery. Include a variety of fruits, vegetables, lean proteins, and whole grains in your meals.
- Supplements: Consult with your doctor about any supplements you might need. Common recommendations include vitamin D, calcium, and iron, which are essential for bone health and overall recovery.
Lifestyle Adjustments:
- Smoking: If you smoke, quitting is imperative. Smoking can impede blood flow and delay healing. Seek support from cessation programs if necessary.
- Alcohol Consumption: Limit alcohol intake before surgery as it can interfere with medications and anesthesia. Follow your doctor’s guidelines on alcohol consumption.
Home Modifications:
- Mobility Aids: Arrange for mobility aids such as crutches, a walker, or a cane to assist you post-surgery. Practice using them before the operation to get comfortable.
- Home Environment: Modify your home to make it more accessible. This might include installing handrails in the bathroom, placing frequently used items within easy reach, and setting up a temporary bedroom on the ground floor to avoid stairs.
Mental Preparation:
- Education: Learn about the surgery, the recovery process, and what to expect. Being informed can reduce anxiety and help you prepare mentally for the journey ahead.
- Support System: Arrange for a support system of family and friends who can assist you during your recovery. Emotional support is just as important as physical assistance.
Preparations with the Doctor
Pre-Surgical Consultation:
- Medical History: Provide a detailed medical history to your surgeon, including any previous surgeries, chronic conditions, and current medications. This information is crucial for planning the procedure and anesthesia.
- Physical Examination: Your doctor will conduct a thorough physical examination, including assessing the range of motion, strength, and stability of your knee joint. Imaging tests such as X-rays or MRIs may be ordered to evaluate the extent of damage and plan the surgery.
Diagnostic Tests:
- Blood Tests: These tests help determine your overall health and detect any underlying conditions that might affect the surgery. Common tests include complete blood count (CBC), electrolyte levels, and blood clotting factors.
- Cardiac Evaluation: If you have a history of heart disease or other cardiovascular issues, a pre-operative cardiac evaluation might be necessary. This can include an electrocardiogram (EKG) or a stress test to ensure your heart is healthy enough for surgery.
Medication Management:
- Review Current Medications: Discuss all medications, including over-the-counter drugs and supplements, with your doctor. Certain medications, such as blood thinners, need to be adjusted or stopped before surgery to prevent complications.
- Pre-Surgery Prescriptions: Your doctor may prescribe medications to take before surgery, such as antibiotics to prevent infection or pain relievers to manage pre-operative pain.
Anesthesia Planning:
- Anesthesia Consultation: Meet with the anesthesiologist to discuss the type of anesthesia that will be used during the surgery. Options include general anesthesia, spinal anesthesia, or regional nerve blocks. The anesthesiologist will explain the risks and benefits of each and help you decide the best option based on your medical history and personal preferences.
Pre-Operative Instructions:
- Fasting: Follow your doctor’s instructions regarding fasting before surgery. Typically, you will be asked not to eat or drink anything after midnight on the night before your surgery.
- Hygiene: You may be instructed to shower with a special antiseptic soap the night before and the morning of your surgery to reduce the risk of infection.
- Clothing: Wear loose, comfortable clothing on the day of surgery. You’ll need to change into a hospital gown upon arrival.
Surgical Logistics:
- Hospital Admission: Confirm the date and time of your surgery, and make arrangements for hospital admission. Ensure you have all necessary documents, including identification, insurance information, and any required forms.
- Transportation: Arrange for transportation to and from the hospital. You will not be able to drive immediately after surgery due to the effects of anesthesia and pain medications.
Post-Surgical Planning:
- Rehabilitation Plan: Discuss the post-surgery rehabilitation plan with your doctor. This will include physical therapy sessions and exercises to aid in your recovery. Knowing the plan in advance helps you prepare mentally and physically.
- Pain Management: Understand the pain management strategy post-surgery. This might include a combination of medications, ice therapy, and relaxation techniques.
Financial Preparations:
- Cost Estimation: Discuss the total cost of the procedure with your healthcare provider, including surgeon fees, hospital charges, anesthesia, and post-operative care. Knowing the financial aspect helps you plan and arrange for necessary payments or insurance claims.
- Insurance Coverage: Verify what your insurance covers and what out-of-pocket expenses you might incur. Ensure all pre-authorization requirements are met to avoid any last-minute surprises.
Additional Considerations
Legal Preparations:
- Advance Directives: Consider setting up advance directives or a medical power of attorney. This ensures your healthcare wishes are followed in case of any unexpected complications during surgery.
Travel Arrangements for Medical Tourists:
- Travel Logistics: If you are traveling from another city or country for your surgery, make all necessary travel arrangements well in advance. This includes flights, accommodation, and local transportation.
- Pre-Travel Health Checks: Ensure you are fit to travel and discuss any potential travel-related health issues with your doctor. Long flights or road trips can pose additional risks, especially if you have other underlying health conditions.
Infection Prevention:
- Pre-Operative Infections: Treat any existing infections before surgery. Even minor infections can delay your surgery and increase the risk of complications. Ensure dental work is completed, as dental infections can be particularly problematic.
- Hygiene Practices: Maintain good personal hygiene and follow all pre-operative cleansing instructions provided by your healthcare team to minimize the risk of surgical site infections.
Psychological Readiness:
- Counseling: Consider psychological counseling if you feel anxious or stressed about the surgery. Talking to a professional can help you manage your fears and prepare mentally for the procedure.
- Support Groups: Joining support groups for knee replacement patients can provide valuable insights and emotional support from others who have undergone the same procedure.
Post-operative Period of Knee Replacement Surgery: Comprehensive Guide to Short-term and Long-term Healing.
Short-Term Healing Period: The First Few Weeks After Surgery
Immediate Post-Operative Care:
- Recovery Room: After the surgery, you will be taken to the recovery room where medical staff will monitor your vital signs, including heart rate, blood pressure, and oxygen levels. This initial phase ensures that you are stable and ready to be moved to your hospital room.
- Pain Management: Pain is a natural part of the recovery process. You will receive pain medications, which may include opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and possibly nerve blocks to manage post-operative pain. Your pain levels will be regularly assessed to adjust medication as needed.
Hospital Stay:
- Duration: The typical hospital stay after knee replacement surgery is about 2-3 days. However, this can vary based on individual health conditions and the type of knee replacement performed.
- Physical Therapy: Physical therapy usually begins within 24 hours of surgery. A physical therapist will guide you through gentle exercises to start regaining mobility in your knee. These exercises are crucial to prevent stiffness and promote blood circulation.
- Mobility and Ambulation: You will be encouraged to get out of bed and start walking with the help of a walker or crutches. Early mobilization is essential to prevent complications such as blood clots and pneumonia.
- Wound Care: Your surgical wound will be monitored and cared for by the medical staff. Instructions on keeping the wound clean and dry will be provided to prevent infection.
Discharge and Home Care:
- Discharge Planning: Before you leave the hospital, you will receive detailed instructions on how to care for your knee at home. This includes guidelines on medications, physical therapy exercises, wound care, and signs of potential complications to watch for.
- Pain Management at Home: You will continue to take pain medications as prescribed. It’s important to follow the dosage instructions and not to skip doses to manage pain effectively.
- Physical Therapy: Continuing physical therapy at home or at a rehabilitation center is crucial. Your therapist will create a tailored exercise program to improve strength, flexibility, and range of motion.
- Activity Restrictions: You will need to avoid certain activities that could strain your knee, such as bending, squatting, and heavy lifting. Gradually increasing your activity level under the guidance of your therapist is essential.
Follow-Up Appointments:
- Initial Follow-Up: Your first follow-up appointment with your surgeon is typically scheduled 1-2 weeks after surgery. During this visit, your wound will be checked, and sutures or staples may be removed. Your progress and pain levels will be assessed.
- Subsequent Visits: Regular follow-up visits will be scheduled to monitor your recovery. These appointments are important to track your progress, address any concerns, and make necessary adjustments to your rehabilitation plan.
Long-Term Healing Period: Months to Years After Surgery
Ongoing Rehabilitation:
- Extended Physical Therapy: Physical therapy often continues for several months post-surgery. The focus will be on advanced exercises to restore full range of motion, strength, and functionality. Therapists will also work on improving your gait and balance.
- Home Exercises: In addition to formal physical therapy sessions, you will be given exercises to perform at home. Consistent adherence to these exercises is vital for optimal recovery.
Gradual Return to Normal Activities:
- Daily Activities: Over time, you will gradually return to your normal daily activities. Tasks such as walking, climbing stairs, and driving can be resumed based on your comfort level and your doctor’s advice.
- Work: The timeline for returning to work varies depending on the nature of your job. Sedentary jobs may be resumed within 4-6 weeks, while physically demanding jobs may require a longer recovery period.
- Recreational Activities: Low-impact activities such as swimming, cycling, and walking are encouraged once your knee has sufficiently healed. High-impact activities like running or jumping should be avoided to prevent damage to the prosthesis.
Long-Term Care and Maintenance:
- Weight Management: Maintaining a healthy weight is crucial to reduce stress on your new knee. Excess weight can lead to increased wear and tear on the prosthesis, potentially shortening its lifespan.
- Healthy Lifestyle: Adopting a healthy lifestyle that includes a balanced diet and regular exercise can enhance your overall well-being and the longevity of your knee replacement.
- Regular Check-Ups: Periodic check-ups with your orthopedic surgeon are important to monitor the condition of your knee replacement. These visits may include X-rays to ensure the prosthesis is functioning properly and detect any issues early.
Managing Potential Complications:
- Infection: While rare, infections can occur long after surgery. Signs of infection include increased pain, redness, swelling, or drainage from the wound. If you suspect an infection, contact your doctor immediately.
- Prosthesis Wear and Tear: Over time, the components of your knee replacement can wear down. Symptoms of wear and tear include increased pain or decreased functionality. Regular monitoring and prompt attention to any changes can help address these issues before they become severe.
- Blood Clots: Continuing to stay active and follow your doctor’s recommendations on blood thinners can help prevent blood clots. Be aware of symptoms such as leg swelling or pain, and seek medical attention if they occur.
Psychological and Emotional Well-being:
- Adjusting to the New Knee: It is normal to experience a range of emotions as you adjust to your new knee. Feelings of frustration or impatience with the recovery process are common. Staying positive and setting realistic expectations can help.
- Support Systems: Engaging with support groups or talking to others who have undergone knee replacement can provide encouragement and practical advice. Mental health professionals can also offer support if you are struggling with the emotional aspects of recovery.
Enhancing Prosthesis Longevity:
- Activity Modification: Avoid activities that place excessive stress on your knee replacement. High-impact sports and heavy lifting should be limited to protect the prosthesis.
- Protecting Your Knee: Wear proper footwear and use assistive devices if needed to prevent falls and protect your knee from injury. Being mindful of your movements and environment can help maintain the integrity of the replacement.
Technological Advances and Future Considerations:
- Advancements in Prosthetics: Stay informed about advancements in knee replacement technology. Innovations in materials and surgical techniques continue to improve outcomes and prosthesis longevity.
- Potential Revisions: While modern knee replacements are designed to last many years, revision surgery may be necessary in the future. Being aware of the signs that indicate a need for revision and maintaining regular follow-ups can help address issues early.
Conclusion.
Navigating the costs and considerations of knee prosthesis installation in Turkey requires careful planning and research.
By understanding the comprehensive pricing details, including factors influencing costs and regional variations, patients can make informed decisions aligned with their medical needs and financial capabilities.
Consulting with reputable orthopedic surgeons, comparing hospital options across different cities, and weighing the benefits of specialized implants versus standard options are critical steps toward achieving successful outcomes in knee replacement surgery.

